Stabilizing Periodontally Compromised Teeth With Fiber Reinforced Composite Resin
 For those patients with moderate-to-severe periodontal disease, tooth mobility can contribute to discomfort when eating and decreased masticatory and occlusal function. Tarnow and Fletcher described the indications and contraindications for splinting periodontally involved teeth.1 They stated that the rationale for splinting teeth should include the severity of periodontal disease as determined by the amount of radiographic bone loss and/or the measured tooth mobility. The literature indicates that the main reasons to reduce tooth mobility with periodontal splinting are primary occlusal trauma, secondary occlusal trauma, and progressive mobility, migration, and pain on function.
For those patients with moderate-to-severe periodontal disease, tooth mobility can contribute to discomfort when eating and decreased masticatory and occlusal function. Tarnow and Fletcher described the indications and contraindications for splinting periodontally involved teeth.1 They stated that the rationale for splinting teeth should include the severity of periodontal disease as determined by the amount of radiographic bone loss and/or the measured tooth mobility. The literature indicates that the main reasons to reduce tooth mobility with periodontal splinting are primary occlusal trauma, secondary occlusal trauma, and progressive mobility, migration, and pain on function.
Primary occlusal trauma is defined as injury resulting from excessive occlusal forces applied to a tooth or teeth with normal periodontal support, while secondary occlusal trauma is injury resulting from normal occlusal forces applied to a tooth or teeth with inadequate periodontal support.
In the past, the splinting of periodontally compromised teeth was contentious. The presumption was that splinting to control tooth mobility was required to control gingival inflammation, periodontitis, and pocket formation. It was assumed that mobility had a direct relationship to attachment loss and formation of vertical osseous defects. Another assumption was that increasing tooth mobility was a direct consequence of traumatic occlusion, bruxism, and clenching. It was suggested that even normal physiologic function, including mastication and swallowing, could contribute to tooth mobility.
Further, it is generally accepted that tooth mobility is an important clinical parameter for predicting tooth prognosis. The reasons to stabilize periodontally compromised teeth include decreased patient discomfort, increased occlusal and masticatory function, and improved prognosis of mobile teeth. Also, regenerative procedures using membranes and bone grafts are far more predictable if tooth movement is eliminated prior to use of a barrier membrane. In cases with mobility that cannot be eliminated by selective coronoplasty alone, splinting should be considered as an adjunct to provide additional tooth stability during the surgical and healing phases of guided tissue regeneration.
 Many different restorative techniques have been used to splint teeth. Before adhesive restorative dentistry was introduced, the optimal choice for splinting teeth was full-coverage cast restorations. A crown was placed on each tooth to be splinted, and the crowns were joined together.One advantage of this technique was that the teeth could be stabilized with an acrylic provisional restoration during periodontal treatment. At the completion of active therapy, the definitive cast restoration was completed. The major drawback of this treatment was that all teeth in the splint were reduced for restoration with crowns. A more conservative approach using a cast restoration on the lingual surfaces of the teeth (a cast gold indirect pin splint) was developed. Later, a modification of this approach—a cast restoration using bonded adhesive resin—was introduced.
Many different restorative techniques have been used to splint teeth. Before adhesive restorative dentistry was introduced, the optimal choice for splinting teeth was full-coverage cast restorations. A crown was placed on each tooth to be splinted, and the crowns were joined together.One advantage of this technique was that the teeth could be stabilized with an acrylic provisional restoration during periodontal treatment. At the completion of active therapy, the definitive cast restoration was completed. The major drawback of this treatment was that all teeth in the splint were reduced for restoration with crowns. A more conservative approach using a cast restoration on the lingual surfaces of the teeth (a cast gold indirect pin splint) was developed. Later, a modification of this approach—a cast restoration using bonded adhesive resin—was introduced.
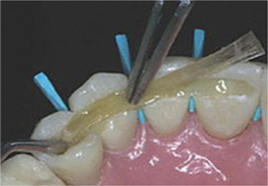
In order to fulfill both the periodontal and restorative needs, ribbons and fibers were developed that could be reinforced with composite resin to form thin-but-strong splints. Both glass fibers and polyethylene fibers have been introduced for this purpose. Glass fibers are treated with a silane chemical coupling agent to allow dental resins to chemically adhere to the glass fiber strands. To improve the bonding of resin to polyethylene fibers, these synthetic polyethylene fibers are chemically treated with thorough surface etching called plasma treatment, which allows the resin to chemically bond to the polyethylene fibers. Without this treatment, there would be no surface wetting of resin and bonding between the 2 substrates. Studies have demonstrated that fiber reinforcement increases the flexural strength and flexural modulus of composite resins. Since all reinforcement fibers provide composite resins with these improved properties, the primary criteria for selection of a particular fiber for use in a periodontal splint are ease of use and availability of an appropriate width. In a multiuser evaluation, ease of use was the primary criterion for selection of a bondable fiber reinforcement. In addition, it has been shown that a woven fiber has an advantage over loose or twisted fibers because it imparts multidirectional reinforcement to polymeric restorative resins.